How laws risk unsafe abortions in India

From time immemorial, women have sought to observe abortion using different methods to terminate pregnancy. Yet, even today not all women enjoy access to safe abortion facilities. The question of the choice of abortion remains hanging in the middle of various debates. When this choice is taken away and women are deprived of the basic right to abortion, the business of unsafe abortion flourishes, as is evident across India.
According to WHO, an unsafe abortion is characterized by the lack or inadequacy of skills of the provider, hazardous techniques or unsanitary facilities.[1] Despite abortion being legal, the high estimated prevalence of unsafe abortion demonstrates a major public health problem in India. Socioeconomic vulnerability and inadequate access to healthcare services combine to leave large numbers of women at risk of unsafe abortion and abortion-related death. The prevalence of unsafe abortion is a profoundly preventable reason for maternal deaths. It can be controlled by giving access to contraception, providing safe abortion facilities and offering treatment in abortion-related complications. Studies as far back as 1981 have demonstrated that when limitations on abortion are eased, the number of deaths because of abortion-related complications is decreased.[2]
Various investigations show lack of legalisation and absence of facilities continue to be the main driving force for women in India to go for unsafe abortions. When women face an unwanted pregnancy, a number of variables impact the decision of choosing an abortion provider and sort of treatment. Shame, stigma, absence of information about safe services available, and a scarcity of trained providers may lead women to seek care from seemingly convenient yet illicit suppliers who use unsafe methods, for example, intrauterine insertion of a remote body (e.g., stick, root, leaf, wire), vaginal abortifacient (e. g., homemade arrangements, mis-prescribed medicines) or sharp curettage.[3] The probability of coming across post-abortion complexities depends on the training and qualification of the abortion provider, the method used and the conditions under which the technique is performed.
Abortion laws in India
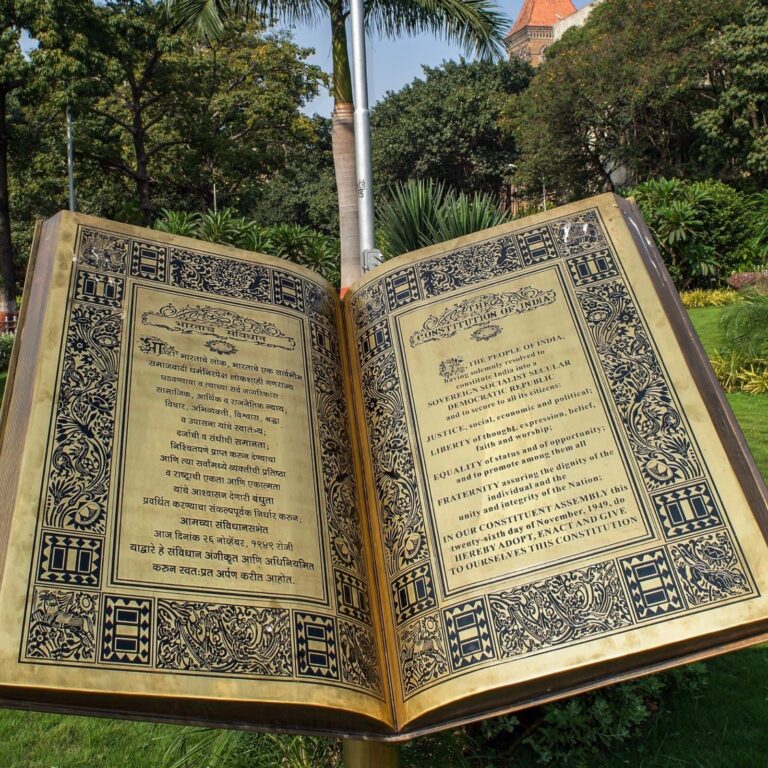
Preceding 1971, abortion was illegal under Section 312 of the Indian Penal Code, 1860, depicting it as purposefully “causing miscarriage”.[4] The law of abortion in India can be traced back to the British enactment of colonial times. The Indian Penal Code 1862 and the Code of Criminal Procedure 1898, with their roots in the British Offenses against the Person Act 1861, made abortion a wrongdoing culpable for both the woman and the abortionist.[5] However, it was allowed to spare the life of the woman.
In the post-colonial period, changes have been made. The progression of abortion law in India started in 1964 with regard to high maternal mortality because of unsafe practices of abortion. The Government of India appointed the Shah Committee to direct an overview of socio-cultural, lawful and clinical aspects pertaining to abortion. In 1966, the Committee suggested the legalisation of abortion to improve women’s health and lives on both empathetic and clinical grounds. The term Medical Termination of Pregnancy (MTP) was used to reduce resistance from socio-religious groups raging against the legalisation of abortion. The MTP Act, passed by Parliament in 1971, legalised abortion in India.[6]
Legal intersections and loopholes
With the introduction of the MTP Act in 1971, liberalization to some extent was seen in abortion law, which was previously illegal under the Indian Penal Code (IPC) of 1860. On meeting various conditions mentioned in the Act, an abortion can be performed.[7] While failing to do so, an abortion would be treated as a crime under a new criminal code namely Bharatiya Nyaya Sanhita, 2023.[8] With time, new laws dealing with other social issues have been passed by the parliament that are often contradictory to the MTP Act, namely the Pre-Conception and Prenatal Diagnostic Techniques (PCPNDT) Act, 1994 and Protection of Children from Sexual Offences (POCSO) Act, 2012.
The Pre-Conception and Prenatal Diagnostic Techniques (PCPNDT) Act, 1994 was enacted to check sex-selective abortion or female foeticide and to create a balance in the sex ratio. The main idea behind this Act was to ban and criminalize the use of sex selection techniques like ultrasound – to stop female foeticide in India. Owing to the fear of getting entangled in a case of female foeticide, medical practitioners started to refuse abortions to pregnant persons. Quite often when a pregnant person wants an abortion, they are denied by medical practitioners to avoid any legal repercussions on mere suspicion that the sex of the fetus has already been determined even when it was not so. Qualified medical practitioners and gynecologists have been guarded in providing abortion services. It has created a sense of fear and insecurity among service providers resulting in another barrier for pregnant people to access safe abortion facilities.[9]
Moreover, a lack of legal awareness and clarity among people as well as medical practitioners creates further gaps in access to reproductive health services. Hence, a genuine case of terminating pregnancy meeting all the conditions of the MTP Act is yet likely to be denied due to legal complications and contradictions with the PCPNDT Act. Such a legal inconsistency furthers the stigmatization of access to reproductive health care and the sexual well-being of the people. It also flourishes non-qualified clandestine abortion facilities with unhygienic and unsafe procedures which is the third leading cause of maternal mortality in India. In other words, close to 8 women die each day due to unsafe abortion practices.[10]
Another law, The Protection of Children from Sexual Offences (POSCO) Act, 2012 is aimed at safeguarding children from sexual abuse, harassment, and exploitation. In its framework, it deals with children below the age of 18 years. The Act has made it mandatory for a service provider to report if the abortion seeker is under the age of 18.[10] While mandatory reporting in itself is not a bad provision, the lack of distinction between consensual and non-consensual cases in the Act becomes a problem. Consequently, a sexual relationship between two people below the age of 18 becomes invalid under the POCSO Act. Failing to report such a case would result in imprisonment of 6 months or a fine or both. Due to mandatory reporting procedures, often medical practitioners refuse to provide abortion services to pregnant women under the age of 18.[12] The problem with this well-intentioned Act is two-fold; firstly, it leads to a complete denial of reproductive rights for adolescents. Secondly, it does not recognize the sexual autonomy of young people. Therefore, it becomes overly controlling and paternalistic in nature. In order to access an abortion facility for people below the age of 18, mandatory reporting under the POCSO Act, along with the provision of consent from a parent or guardian under the MTP Act, is a point of intersection between the two Acts, which often complicates and delays in accessing safe abortion services.
Way forward
While these well-intentioned laws passed by the parliament provide legislative protection, the contentions of the same laws often lead to hindrances and delays in access to healthcare services among younger people. Giving absolute powers to police or medical practitioners would be even more unfavourable to achieving a just and speedy reproductive healthcare system. It is important that such legal loopholes are addressed with nuanced discussions around the highly stigmatized subject of abortion in Indian society. Besides legal complexities, abortion has socio-cultural and health implications. It is as much a social as it is a health or legal matter. Therefore, we need a broader perspective and a comprehensive rights-based approach to address the problem. To tackle socio-cultural aspects, raising awareness about abortion through early sexual and reproductive health education may help in destigmatizing abortion not only for the general public but also for medical practitioners.[13] Educating people about the use of different contraceptive methods would help to prevent unwanted pregnancies resulting in unsafe abortions, particularly in rural India. It requires improvement in family planning services and policy interventions.
References
- WHO (1993), The Prevention and Management of Unsafe Abortion, Division of Family Health, World Health Organisation, p. 03.
- Henshaw, S. K. (1990), Induced Abortion: A World Review, Family Planning Perspectives, Guttmacher Institute, Vol. 22, No. 2 pp. 76-89.
- Singh, S. et. al. (2015), Abortion and Unintended Pregnancy in Six Indian States: Findings and Implications for Policies and Programs, Guttmacher Institute
- Indian Penal Code (1860), ss 312-316
- Hirve, S. S. (2004), Abortion Law, Policy and Services in India: A Critical Review, Reproductive Health Matters, Vol. 12, No. 24, Supplement: Abortion Law, Policy and Practice in Transition, pp. 114-121
- Banerjee, Sushanta K. and Andersen K. (2012), Exploring the pathways of unsafe abortion in Madhya Pradesh, India, Global Public Health, Vol. 7, No. 8, 882 896
- The Medical Termination of Pregnancy Act, (1971), ss 3-4
- Bharatiya Nyaya Sanhita (2023), ss 88-92
- Chandra, A. et. al. (2021), Legal Barriers to Accessing Safe Abortion Services in India: A Fact Finding Study, Center for Reproductive Rights, p. 30
- Baker, D. et. al. (2022), The State of World Population (SoWP), United Nations Population Fund (UNFPA)
- The Protection of Children from Sexual Offences Act, (2012), ss 19-23
- Chandra, A. et. al. (2021), Legal Barriers to Accessing Safe Abortion Services in India: A Fact Finding Study, Center for Reproductive Rights, p. 30
- Singh, G. (2024, Oct 07) We Need to Talk More About Abortion Care in India, The Wire. Retrieved November 27, 2024, from https://thewire.in/health/abortion-health-women-social-issue-contraceptives